Sensory issues are a core part of Autism Spectrum Disorder (ASD), affecting how an individual’s brain processes information from their senses. For a person with autism, the world can feel overwhelming, under-stimulating, or both. These differences are not a choice or a behavioral issue; they are rooted in how the individual’s brain is wired to receive and process sensory information. Understanding these neurological differences is the first step toward providing effective support, as it allows for compassionate and effective intervention strategies.
Understanding the Types of Sensory Responses
Sensory processing can manifest in three main ways, with most people on the spectrum experiencing a mix of these depending on the situation and their current state of well-being. A 2017 study in the journal Frontiers in Human Neuroscience found that autistic individuals show a greater neural response to sensory stimuli, providing a biological basis for hypersensitivity. This scientific backing helps us move beyond simple observation to a deeper understanding of the challenges many individuals face. It’s crucial for caregivers and educators to recognize that these responses are involuntary and require patience and support, not punishment or judgment.
1. Hypersensitivity (Over-Responsiveness)
This is when an individual’s brain processes sensory input as stronger or more intense than it is. It can feel painful, overwhelming, or unbearable, often leading to sensory avoidance. An example of this is a child who covers their ears and cries at the sound of a vacuum cleaner because the noise feels physically painful to them. Similarly, bright fluorescent lights can cause headaches and distress, prompting them to seek out dim environments or wear sunglasses indoors, even on a cloudy day.
Strategies & Tips:
Auditory: Provide noise-canceling headphones or earplugs. Give a heads-up before entering noisy places. Create a “quiet zone” at home or school.
Visual: Use sunglasses or a wide-brimmed hat outdoors. Replace fluorescent bulbs with softer lighting. Use a visor or “tunnel” in a shopping cart to limit visual clutter.
Tactile: Cut tags out of clothing and choose soft, seamless fabrics. Allow the individual to dress themselves to have control over the texture. Warn them before you touch them, and use firm pressure instead of light touch.
2. Hyposensitivity (Under-Responsiveness)
This is when the brain does not register sensory input strongly enough, or it takes a longer time to process it. This can lead to a constant need for more intense input to feel regulated. A child with hyposensitivity may not notice a scraped knee or may seem unaware of a sudden, loud noise that startles others. Because their body craves more intense input, they might frequently bump into objects or have a higher tolerance for pain compared to their peers.
- Strategies & Tips:
- Touch/Proprioception: Encourage activities with deep pressure, like tight hugs, weighted blankets, or “squeezing” games. Use resistance bands or heavy work tasks, like pushing a laundry basket or carrying heavy books.
- Oral: Offer crunchy foods (carrots, pretzels), chewy items (licorice, gum), or a chewy necklace to provide oral input.
- General Awareness: Use a visual schedule or set timers for routines like brushing teeth to ensure they are completed even if the individual doesn’t “feel” the need to do so.

3. Sensory Seeking
This is an active craving for sensory stimulation to help the body feel regulated and calm. It is a conscious or unconscious attempt to “feed” the sensory system that is under-responsive. For instance, a person might constantly rock in their chair or chew on the end of their pen to provide their brain with the movement and oral input it is craving. These behaviors are not without purpose; they are a form of self-regulation that helps an individual manage their internal state and cope with their environment.
- Strategies & Tips:
- Movement: Provide safe outlets for movement, such as a mini-trampoline, a sensory swing, or a therapy ball to sit on instead of a chair. Schedule movement breaks throughout the day.
- Fidgets: Offer a variety of appropriate fidget toys (e.g., squishy balls, fidget spinners, tactile cubes) to provide a safe and acceptable way to get sensory input.
- Visual: Provide lava lamps, glitter bottles, or a “sensory bin” filled with different textures to satisfy visual and tactile seeking.
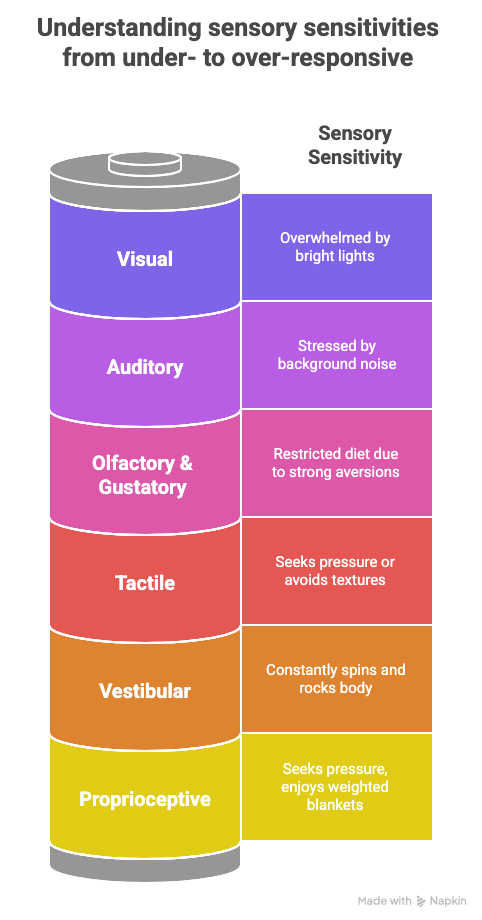
The Eight Sensory Systems
To fully understand sensory issues, we must look beyond the five basic senses. Individuals with autism can experience differences in all eight sensory systems, which the American Occupational Therapy Association (AOTA) and other expert organizations have extensively researched. This comprehensive view is essential because a person’s sensory profile is unique and often involves a complex interplay between multiple systems. Understanding all eight systems allows for a more personalized and effective approach to sensory support.
- Interoception: This is the internal sense of what’s happening inside a person’s body, such as hunger, thirst, or pain. According to a study in Frontiers in Psychology, differences in interoception can make it difficult for individuals with autism to recognize and respond to their body’s internal signals, which can be a significant health and safety concern.
- Strategies & Tips: Use visual prompts for bodily needs (e.g., a picture of a glass of water to prompt drinking). Set reminders for bathroom breaks and mealtimes. Use a body check chart to help the individual identify and name internal feelings.
The Impact on Daily Life
Sensory issues aren’t just a minor annoyance; they significantly impact an individual’s emotional well-being and ability to navigate the world. Sensory overload can cause intense stress, anxiety, meltdowns, or shutdowns (a complete withdrawal from the environment and communication). It’s important to recognize these reactions as a natural response to an overwhelming situation, rather than a misbehavior. This understanding helps foster empathy and provides the foundation for creating sensory-friendly environments that are crucial for an individual’s mental and physical health.
- Stimming as a Coping Mechanism: Repetitive behaviors like hand-flapping or rocking (known as stimming) are a person’s way of self-regulating and coping with overwhelming sensory input. As noted by Dr. Stephen Porges, creator of the Polyvagal Theory, these behaviors can help calm a dysregulated nervous system in response to overwhelming sensory input. When an individual is forced to suppress their stims, it can lead to increased anxiety and a greater risk of sensory overload, highlighting the importance of allowing for these natural coping mechanisms.
How ABA Therapy Helps with Sensory Challenges
Applied Behavior Analysis (ABA) and Occupational Therapy (OT) are two evidence-based approaches that can work together to help individuals manage and adapt to sensory challenges. These therapies don’t aim to “cure” sensory differences but rather to provide the individual with tools and strategies to navigate a sensory world that wasn’t designed for them. By taking a collaborative and interdisciplinary approach, therapists can address both the behavioral responses and the underlying sensory needs of an individual.
-
Applied Behavior Analysis (ABA)
ABA focuses on understanding how sensory issues affect behavior and teaches practical coping skills through evidence-based techniques. “ABA therapy is a highly individualized approach,” says [Author’s Name], a Board Certified Behavior Analyst (BCBA) with over 10 years of experience. “We first identify the function of a behavior—whether it’s seeking sensory input or escaping it—and then teach a more appropriate way to meet that need.” For instance, a therapist might teach a child to use a “sensory toolbox” with items like fidget spinners, stress balls, or a weighted blanket to help them self-regulate in different environments, providing a proactive solution to a potential meltdown.
- Specific ABA Strategies:
- Functional Communication Training: Teach the individual to use words or pictures to ask for a break or say “too loud.”
- Positive Reinforcement: Reward calm behaviors in a sensory-challenging environment (e.g., praising a child for tolerating a loud sound for a specific amount of time).
- Systematic Desensitization: Gradually introduce a feared sensory stimulus while the individual is calm and relaxed, pairing it with a preferred activity to build tolerance.
Occupational Therapy (OT)
OT often focuses directly on sensory integration and provides tools and activities to help the nervous system become more regulated. OT practitioners use a sensory integration approach, which, according to research from the American Occupational Therapy Association (AOTA), can help improve a person’s ability to process and organize sensory input. An OT can design a “sensory diet,” a daily schedule of sensory-based activities like jumping on a trampoline or using a therapy ball, to help a person stay regulated throughout the day. This proactive approach helps prevent sensory overload before it occurs, improving overall quality of life and participation in daily routines.
Check Out Our Sarjapur Autism Treatment Center Location : https://share.google/iuB30wEakc4v0mU53
- Specific ABA Strategies:
This journey is not one that any parent has to walk alone. There are professionals, advocates, and communities dedicated to supporting families of children with autism. Sharing experiences, learning from others, and staying informed about the latest tools and strategies can empower parents to face challenges with confidence.
References
- Autism Speaks: https://www.autismspeaks.org/sensory-issues
- The National Autistic Society (UK): https://www.autism.org.uk/advice-and-guidance/topics/sensory-differences
- The American Occupational Therapy Association (AOTA): https://www.aota.org/about-occupational-therapy/professionals/children-and-youth/autism
- Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/sensory-processing-disorder-spd
Resources
- Autism Support Group : https://www.facebook.com/groups/SupportAutism
- Youtube Podcast : https://www.youtube.com/@BeChangeCenter
- Behavior Analyst Certification Board (BACB): www.bacb.com
- Instagram : https://www.instagram.com/bechangeaba/